Hemorrhoids are a common yet often misunderstood condition that affects millions of people worldwide.
Despite their prevalence, many hesitate to talk about the discomfort they cause, leaving people unsure of what to expect.
If you’ve ever experienced itching, burning, or pain near your anus, you might be wondering: what does a hemorrhoid feel like?
Understanding the sensations associated with hemorrhoids is the first step toward identifying the problem and finding effective relief.
Hemorrhoids can be internal, forming inside the rectum, or external, appearing as swollen lumps under the skin around the anus.
Each type comes with distinct symptoms, ranging from mild discomfort to sharp pain.
This guide will help you recognize the signs, understand the causes, and explore treatment options, empowering you to take control of your health and reduce discomfort before it escalates.
What Are Hemorrhoids?
Hemorrhoids are swollen veins located in the lower rectum or around the anus, similar to varicose veins that appear in the legs. They occur when the blood vessels in this area become stretched or inflamed, often due to increased pressure. While they are common and usually not life-threatening, hemorrhoids can cause discomfort, irritation, and in some cases, bleeding.
There are three main types of hemorrhoids:
- Internal hemorrhoids – These form inside the rectum and are usually painless. They may go unnoticed for a long time but can cause bleeding during bowel movements. In some cases, internal hemorrhoids can prolapse, or extend outside the anus, leading to discomfort.
- External hemorrhoids – These develop under the skin around the anus and are often more noticeable. They can cause itching, swelling, and pain, especially when sitting or during bowel movements.
- Thrombosed hemorrhoids – These occur when a blood clot forms inside an external hemorrhoid, causing severe pain, swelling, and a bluish lump near the anus.
Several factors contribute to the development of hemorrhoids, including chronic constipation or diarrhea, straining during bowel movements, pregnancy, prolonged sitting, and a low-fiber diet. Aging can also weaken veins in the rectal area, making hemorrhoids more likely.
Understanding the types and causes of hemorrhoids is essential for recognizing symptoms early and seeking appropriate treatment. By knowing the difference between internal, external, and thrombosed hemorrhoids, you can better manage discomfort and prevent complications.
Symptoms: What Does a Hemorrhoid Feel Like?
Hemorrhoids can cause a variety of sensations, and the symptoms often depend on whether the hemorrhoid is internal, external, or thrombosed. Understanding these differences is key to identifying the condition early.
Internal hemorrhoids form inside the rectum and are usually painless at first. Many people only notice them when they cause bright red bleeding during bowel movements. You might also experience a sensation of fullness or pressure in the rectum, or notice mucus discharge. In some cases, internal hemorrhoids can prolapse, meaning they extend outside the anus, which can cause mild discomfort or irritation.
External hemorrhoids, found under the skin around the anus, are often more noticeable and uncomfortable. They can cause itching, swelling, and soreness, and sometimes produce a painful lump that becomes more tender when sitting or during bowel movements. Many people describe a burning or sharp pain associated with external hemorrhoids, especially if inflammation is present.
A thrombosed hemorrhoid occurs when a blood clot forms within an external hemorrhoid. This condition can cause sudden, severe pain, a hard lump near the anus, and sometimes a bluish or purplish discoloration.
Other common sensations include irritation, burning after bowel movements, and general discomfort in the anal area. While the pain varies in intensity, even mild symptoms can affect daily life and make sitting or exercising uncomfortable.
Recognizing these symptoms early allows for timely management and relief, whether through home remedies, lifestyle changes, or medical treatment. Understanding what a hemorrhoid feels like is the first step toward preventing further complications.
Causes and Risk Factors
Hemorrhoids develop when the veins in the rectal and anal area become swollen or inflamed due to increased pressure. While anyone can develop hemorrhoids, certain behaviors, conditions, and lifestyle factors make them more likely. Understanding these causes can help you prevent or manage them effectively.
Straining during bowel movements is one of the most common causes. Chronic constipation forces extra pressure on the rectal veins, which can lead to swelling over time. Similarly, frequent diarrhea can irritate and inflame the anal area, increasing the risk of hemorrhoids.
Pregnancy and childbirth are also significant factors. The growing uterus puts pressure on the veins in the pelvic region, and the strain during labor can trigger hemorrhoids.
Lifestyle factors play a role as well. Sitting or standing for long periods, particularly on hard surfaces, increases pressure on the anal veins. A low-fiber diet can cause harder stools, making bowel movements more difficult and straining more likely. Lack of regular exercise can also contribute to constipation, increasing the risk.
Other risk factors include aging, as veins lose elasticity over time, and genetics, which can make some people more prone to hemorrhoids. Obesity, heavy lifting, and certain medical conditions affecting bowel habits can also contribute.
By identifying these causes and risk factors, you can take preventive measures, such as improving diet, staying active, and practicing healthy bathroom habits. Awareness is key to minimizing discomfort and reducing the likelihood of hemorrhoid flare-ups.
How Hemorrhoids Are Diagnosed
Recognizing the symptoms of hemorrhoids is important, but a proper diagnosis ensures that the discomfort is not caused by another condition, such as anal fissures, infections, or more serious colorectal issues. Doctors typically use a combination of symptom evaluation and physical examination to diagnose hemorrhoids accurately.
For external hemorrhoids, diagnosis is often straightforward. A visual inspection of the anal area can reveal swollen veins, lumps, or discoloration. Patients may report pain, itching, or bleeding, which helps the doctor confirm the condition.
Internal hemorrhoids, located inside the rectum, are not visible externally, so doctors may use additional methods. A digital rectal exam involves gently inserting a gloved finger into the rectum to feel for swelling or prolapsed tissue. In some cases, an anoscopy a small, tube-like instrument with a light may be used to examine the rectal lining more closely. This helps determine the size, location, and severity of the hemorrhoids.
Doctors may also ask about your bowel habits, diet, and lifestyle to identify possible causes and contributing factors. Reporting symptoms such as bright red bleeding, mucus discharge, or persistent pain helps guide the diagnosis.
Early diagnosis is important because it allows for timely management and reduces the risk of complications. Once the type and severity of hemorrhoids are confirmed, healthcare providers can recommend appropriate home remedies, lifestyle changes, or medical treatments to relieve discomfort and prevent recurrence.
Treatment Options
Hemorrhoids can often be managed effectively with a combination of home remedies, lifestyle changes, and medical treatments, depending on their type and severity.
Home remedies are usually the first line of relief. Sitz baths, where you soak the anal area in warm water for 10–15 minutes, can reduce swelling and soothe discomfort. Over-the-counter creams or ointments containing witch hazel or hydrocortisone can help relieve itching and inflammation. Applying cold compresses to the affected area can also reduce swelling and pain.
Lifestyle adjustments play a crucial role in preventing flare-ups. Eating a high-fiber diet with plenty of fruits, vegetables, and whole grains softens stools and reduces straining during bowel movements. Staying hydrated and exercising regularly supports healthy digestion. Avoiding prolonged sitting or standing and practicing proper bathroom habits, like not delaying the urge to go, can further prevent hemorrhoid development.
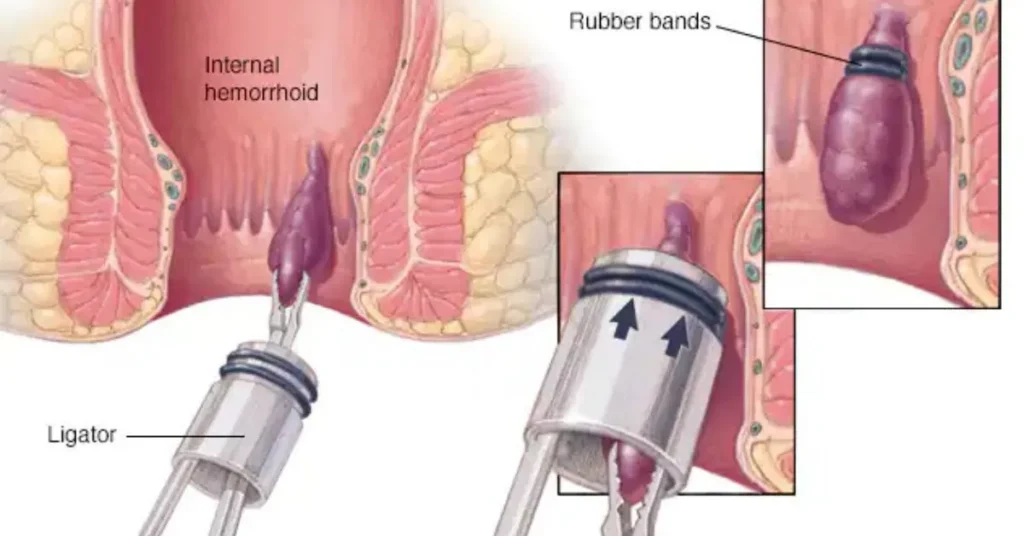
When home remedies are insufficient, medical treatments may be necessary. Minimally invasive procedures include rubber band ligation, which cuts off blood supply to internal hemorrhoids, and sclerotherapy, which shrinks hemorrhoids with a special solution. In more severe cases, infrared coagulation or surgical removal (hemorrhoidectomy) may be recommended.
Pain management is also important. Over-the-counter pain relievers like acetaminophen or ibuprofen can reduce discomfort.
With early treatment and consistent care, most hemorrhoids improve within a few days to weeks. Understanding the available options empowers you to relieve symptoms, prevent recurrence, and maintain comfort in daily life.
Prevention Tips
Preventing hemorrhoids is often easier than treating them, and making small lifestyle adjustments can significantly reduce the risk of flare-ups. Most prevention strategies focus on reducing pressure on the rectal veins and maintaining healthy bowel habits.
Increase dietary fiber by including more fruits, vegetables, whole grains, and legumes in your meals. Fiber softens stools, making them easier to pass and reducing the need to strain during bowel movements. Pair this with adequate hydration, as drinking plenty of water keeps stools soft and helps maintain regularity.
Exercise regularly to improve digestion and circulation, which can prevent constipation and reduce pressure on anal veins. Even light activities like walking or yoga can make a noticeable difference.
Practice healthy bathroom habits. Avoid straining, holding your breath, or spending long periods sitting on the toilet. Respond promptly to bowel urges rather than delaying them, which can contribute to constipation and hemorrhoid development.
Avoid prolonged sitting or standing, especially on hard surfaces. Taking short breaks to move around can relieve pressure on the veins in the lower rectum.
Other helpful strategies include maintaining a healthy weight, avoiding heavy lifting when possible, and using a cushion or soft surface if sitting for long periods is unavoidable.
By incorporating these simple habits into your daily routine, you can reduce the likelihood of developing hemorrhoids and minimize discomfort if they occur. Prevention is the most effective strategy for long-term relief and overall digestive health.
When to See a Doctor
While most hemorrhoids can be managed at home with lifestyle changes and over-the-counter remedies, there are times when professional medical care is essential. Knowing when to see a doctor ensures proper treatment and prevents potential complications.
Seek medical attention if you experience severe or persistent pain. External hemorrhoids can sometimes become thrombosed, forming a blood clot that causes intense, sudden discomfort. Pain that does not improve with home remedies may indicate a more serious problem requiring medical intervention.
Excessive or recurring bleeding during bowel movements is another red flag. While minor bleeding from internal hemorrhoids is common, frequent or heavy bleeding can indicate complications or other underlying conditions, such as anal fissures or colorectal issues.
A lump that does not improve or continues to grow should also be evaluated by a healthcare professional. This could be a thrombosed hemorrhoid or another medical condition that requires treatment.
Other warning signs include signs of infection, such as swelling, redness, pus, or fever. Additionally, if you experience changes in bowel habits, unexplained weight loss, or severe discomfort, it’s important to rule out more serious gastrointestinal conditions.
Early consultation with a doctor allows for accurate diagnosis and treatment options, which may include prescription medications, minimally invasive procedures, or, in severe cases, surgery. Timely medical care not only relieves symptoms but also reduces the risk of complications and improves overall quality of life.
Living With Hemorrhoids
Living with hemorrhoids can be uncomfortable, but with the right strategies, you can manage symptoms and maintain daily comfort. The key is combining proper self-care, lifestyle adjustments, and awareness of triggers.
Managing discomfort begins with hygiene. Gently cleaning the anal area after bowel movements with warm water or unscented wipes can reduce irritation and prevent itching. Avoid harsh soaps or rubbing the area, as this can worsen inflammation. Sitz baths are a simple and effective way to relieve swelling and soothe pain, especially during flare-ups.
Diet and hydration continue to play a major role in symptom management. Eating a high-fiber diet and drinking plenty of water can prevent constipation, reduce straining, and minimize pressure on the anal veins. Softening stools makes bowel movements less painful and lowers the risk of aggravating hemorrhoids.
Daily routines can also make a difference. Avoid sitting for long periods, take breaks to move around, and use cushions if necessary. Exercise regularly to improve circulation and overall digestive health.
It’s important to recognize and manage flare-ups early. Over-the-counter creams, cold compresses, and gentle pain relievers can help during periods of discomfort. Keep track of triggers such as prolonged sitting, heavy lifting, or low-fiber meals to prevent recurring episodes.
Finally, don’t hesitate to consult a healthcare professional if symptoms persist or worsen. With consistent care and awareness, most people can live comfortably with hemorrhoids, minimizing discomfort and preventing serious complications.
Conclusion
Hemorrhoids are a common and often uncomfortable condition that can affect anyone, yet they are manageable with the right knowledge and care.
Understanding what a hemorrhoid feels like is the first step toward effective relief. Whether internal, external, or thrombosed, recognizing the symptoms such as itching, swelling, pain, burning, or bleeding helps you take timely action and prevents complications.
Prevention is equally important. Simple lifestyle adjustments, including a high-fiber diet, adequate hydration, regular exercise, and healthy bathroom habits, can significantly reduce the risk of developing hemorrhoids or experiencing flare-ups.
Avoiding prolonged sitting or standing and managing bowel habits carefully further supports long-term comfort.
Treatment options range from home remedies like sitz baths, cold compresses, and over-the-counter creams, to medical interventions for more severe cases.
Early diagnosis and proper care can relieve symptoms quickly and improve quality of life.
Most importantly, while hemorrhoids can be painful or irritating, they are usually not dangerous.
However, persistent pain, excessive bleeding, or unusual lumps should always be evaluated by a healthcare professional to rule out other conditions and ensure appropriate treatment.
By understanding the causes, symptoms, and treatment options, you can take control of your health, reduce discomfort, and live comfortably.
Awareness, prevention, and timely care are the keys to managing hemorrhoids effectively, allowing you to maintain confidence and comfort in daily life.

Jordon Fox is an emerging artist and creative from Philadelphia, Pennsylvania, known for blending music, fashion, and fitness into his personal brand and artistic identity. He’s built a reputation as a multi-talented creator with a strong focus on authenticity and inspiring others.