If you’ve ever felt a sharp pain, burning sensation, tingling, or numbness that seems to come out of nowhere, you might wonder, “What does a pinched nerve feel like?”
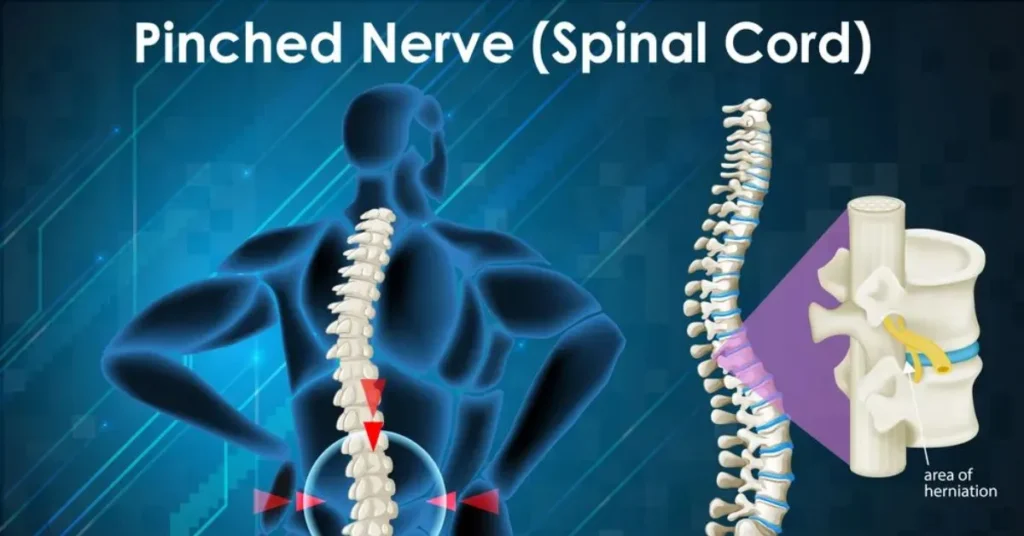
A pinched nerve happens when too much pressure is placed on a nerve by surrounding tissues such as bones, muscles, tendons, or cartilage. This pressure disrupts normal nerve function, leading to pain and other uncomfortable sensations that can range from mild to severe.
Pinched nerve symptoms often feel different from ordinary muscle pain. The discomfort may travel to other parts of the body, feel like an electric shock, or cause weakness in your arm, hand, leg, or foot. These symptoms can be alarming, especially if they interfere with daily activities or sleep.
Understanding how a pinched nerve feels, what causes it, and when it may be serious can help you decide the right next steps. This guide explains the sensations, symptoms, and signs to watch for.
What Is a Pinched Nerve?
A pinched nerve occurs when a nerve is compressed, irritated, or squeezed by surrounding tissues such as bones, muscles, tendons, ligaments, or cartilage. Nerves act as communication pathways between the brain and the rest of the body, carrying signals that control movement, sensation, and pain. When pressure is placed on a nerve, these signals are disrupted, which leads to discomfort and other noticeable symptoms.
This compression often happens in areas where nerves travel through narrow spaces, such as the spine, neck, wrist, or elbow. For example, a bulging or herniated disc in the spine can press against nearby nerves, while repetitive motions or poor posture can cause muscles and tendons to tighten and irritate a nerve. Conditions like arthritis may also lead to bone spurs that narrow nerve pathways over time.
The severity of a pinched nerve can vary. In mild cases, symptoms may come and go and improve with rest or changes in activity. In more severe or prolonged cases, constant pressure can cause ongoing pain, numbness, or muscle weakness. If left untreated for long periods, nerve compression may even lead to long-term nerve damage.
Understanding what a pinched nerve is helps explain why the symptoms can feel unusual or intense compared to typical muscle pain. Because nerves affect sensation and movement, even a small amount of pressure can trigger significant discomfort, making early recognition and proper care important.
What Does a Pinched Nerve Feel Like?
A pinched nerve can cause a wide range of sensations, and the experience often feels different from common aches or muscle soreness. One of the most noticeable symptoms is sharp or stabbing pain that may appear suddenly or worsen with certain movements. This pain is often described as intense and localized, but it can also travel along the path of the affected nerve.
Many people report a burning or searing sensation, especially when the nerve is irritated for a long time. Another common feeling is tingling or “pins and needles,” similar to the sensation you get when a limb falls asleep. This tingling may come and go or remain constant, depending on how much pressure is on the nerve.
Numbness is also a key sign of a pinched nerve. You may notice reduced sensation or a “dead” feeling in the affected area, such as the fingers, toes, or part of the arm or leg. In some cases, the nerve may send signals that feel like electric shocks, particularly when you move, cough, or change position.
A pinched nerve can also affect muscle function. Muscle weakness, heaviness, or difficulty gripping or lifting objects may occur if the nerve controls muscle movement. Unlike muscle pain, these symptoms often spread beyond one spot and may worsen at night or after repetitive activity. Because nerve pain behaves differently, recognizing these sensations can help identify a pinched nerve early.
Pinched Nerve Symptoms by Body Location
The symptoms of a pinched nerve can vary depending on where the nerve compression occurs. Because nerves travel from the spine to different parts of the body, pain and other sensations often appear far from the actual source of the problem.
A pinched nerve in the neck (cervical spine) commonly causes neck pain and stiffness along with symptoms that radiate into the shoulder, arm, or hand. You may experience tingling, numbness, or weakness in the fingers, and in some cases, headaches can develop due to nerve irritation.
When a pinched nerve affects the shoulder, pain may worsen when lifting or rotating the arm. This can be accompanied by arm weakness, burning sensations, or tingling that travels downward.
A pinched nerve in the arm or elbow, such as with cubital tunnel syndrome, often leads to numbness or tingling in the forearm and fingers, especially the ring and little finger. Grip strength may decrease, making it harder to hold objects.
In the wrist or hand, nerve compression like carpal tunnel syndrome causes numbness, tingling, or pain in the thumb, index, and middle fingers. Symptoms frequently worsen at night.
A pinched nerve in the lower back can cause localized back pain along with stiffness and muscle spasms. When the sciatic nerve is involved, pain may shoot down the leg, causing burning, electric sensations, or numbness in the thigh, calf, or foot. Understanding symptom location helps identify the affected nerve.
Pinched Nerve vs Muscle Pain
One of the most confusing aspects of a pinched nerve is that its symptoms can feel similar to muscle pain. However, understanding the differences can help you identify the underlying cause and take appropriate action.
Pain Type: Muscle pain is usually dull, achy, or sore and often worsens with movement or after physical activity. In contrast, a pinched nerve often causes sharp, stabbing, or burning pain that can radiate from the source to other areas, following the nerve’s path. For example, a pinched nerve in the neck may produce pain that shoots down the arm, which is uncommon with ordinary muscle soreness.
Tingling and Numbness: Muscle pain rarely causes tingling, numbness, or a “pins and needles” sensation. These are classic signs of nerve involvement. If you notice electrical or prickling sensations in addition to pain, a nerve is likely affected.
Weakness: While muscle fatigue can occur with overuse, true muscle weakness difficulty gripping, lifting, or controlling certain movements is more characteristic of a pinched nerve. Muscle pain alone usually doesn’t impair function to this extent.
Symptom Spread: Muscle pain tends to stay localized to the affected area, whereas nerve pain may radiate along a limb or into distant regions, following the nerve’s pathway.
Response to Rest: Muscle pain typically improves with rest and gentle stretching. Nerve pain may persist or worsen with certain positions, movements, or even at night.
What Causes a Pinched Nerve?
A pinched nerve can develop for many reasons, often related to pressure, injury, or structural changes in the body. Understanding the causes can help prevent symptoms or reduce their severity.
One of the most common causes is poor posture. Sitting or standing incorrectly for long periods especially with a slouched back or forward-leaning neck can compress nerves in the spine. Repetitive movements, such as typing, lifting, or certain sports activities, can also irritate nerves over time.
Injury or trauma is another frequent cause. Accidents, falls, or sudden impacts can shift bones, discs, or soft tissues, putting pressure on nearby nerves. Herniated or bulging discs in the spine are a particularly common culprit, as they can press directly against nerve roots. Bone spurs, often caused by arthritis, may narrow spaces through which nerves pass, leading to chronic compression.
Other factors include obesity and pregnancy, which increase pressure on the spine or joints, and conditions that cause inflammation or swelling around nerves. Tight muscles, tendons, or ligaments can also pinch a nerve when they press against it repeatedly.
Certain lifestyle habits can make pinched nerves more likely. Sedentary behavior, lack of stretching, and carrying heavy loads improperly can all contribute to nerve compression over time.
Pinched nerves can range from mild and temporary to severe and chronic. Identifying and addressing the underlying cause whether through posture correction, exercise, or medical treatment is key to reducing discomfort and preventing long-term nerve damage.
How Long Does a Pinched Nerve Last?
The duration of a pinched nerve can vary widely depending on its severity, location, and the underlying cause. For many people, mild cases improve within a few days to a few weeks with rest, gentle movement, and simple home care. These temporary episodes often occur when a nerve is compressed by muscle tension, minor injury, or brief repetitive movements.
Moderate or more persistent cases may last several weeks to a few months, particularly if the nerve is compressed by structural issues such as a herniated disc, bone spur, or chronic poor posture. During this time, symptoms like tingling, numbness, and intermittent pain may fluctuate. Some people notice that their discomfort worsens after certain activities, long periods of sitting, or at night, while improving with proper posture, stretching, or supportive therapy.
In severe or untreated cases, a pinched nerve can become chronic, lasting months or even longer. Prolonged nerve compression may lead to ongoing pain, muscle weakness, or permanent nerve damage if not addressed promptly. This is why early recognition and management are crucial.
Several factors influence recovery time, including age, overall health, activity level, and whether conservative treatments or medical interventions are applied. Maintaining proper posture, avoiding repetitive strain, and performing recommended stretches can speed recovery and reduce recurrence. In some cases, physical therapy, medications, or minor procedures may be necessary to relieve pressure on the nerve.
Understanding the typical timeline helps set realistic expectations and encourages early treatment to prevent prolonged discomfort or complications.
When Is a Pinched Nerve Serious?
While many pinched nerves improve on their own, certain symptoms indicate a more serious problem that requires immediate medical attention. Recognizing these red flags is essential to prevent permanent nerve damage or complications.
One major warning sign is progressive or severe muscle weakness. If the affected limb suddenly feels weak, heavy, or difficult to control such as dropping objects, struggling to grip, or having trouble walking it may indicate that the nerve is under significant pressure. Similarly, loss of sensation or severe numbness in an arm, hand, leg, or foot can suggest that the nerve is being compressed for an extended period, potentially causing lasting damage.
Another critical symptom is loss of bladder or bowel control, which can occur if nerves in the lower spine are severely compressed. This is a medical emergency and requires immediate evaluation. Persistent, intense pain that does not improve with rest, stretches, or pain relief is also a warning sign. Pain that radiates rapidly down a limb or is accompanied by tingling and burning sensations that worsen over time may indicate nerve irritation that should be addressed promptly.
Certain situations also increase urgency, such as pinched nerves caused by trauma, herniated discs, or underlying conditions like arthritis or spinal stenosis. People experiencing sudden, unexplained weakness, loss of function, or severe pain should seek professional care immediately.
Early intervention can prevent long-term nerve damage, restore function, and relieve discomfort. Even if symptoms seem mild initially, monitoring changes in strength, sensation, and pain intensity is crucial for determining when medical attention is necessary.
How Is a Pinched Nerve Diagnosed?
Diagnosing a pinched nerve begins with a detailed medical history and physical examination. A doctor will ask about your symptoms, their onset, location, intensity, and whether certain movements or positions worsen the discomfort. They will also inquire about lifestyle factors, injuries, and previous health conditions that could contribute to nerve compression.
During the physical exam, a healthcare professional will assess strength, sensation, reflexes, and range of motion. Tests may include asking you to move your arms, legs, or neck in specific ways to see if pain, tingling, or numbness occurs. The doctor may also tap on certain nerves or gently apply pressure to detect areas of sensitivity, which helps identify the affected nerve.
If further confirmation is needed, imaging tests such as X-rays, MRI, or CT scans may be ordered. These can reveal structural issues like herniated discs, bone spurs, or spinal stenosis that may compress nerves. Nerve conduction studies and electromyography (EMG) are additional tools used to measure how well electrical signals travel through the nerves and muscles. These tests can pinpoint the exact location and severity of nerve compression.
Diagnosis is essential for determining the appropriate treatment plan. Mild cases may only require rest, posture adjustments, or stretches, while severe or persistent cases may need medications, physical therapy, or even surgical intervention. Early and accurate diagnosis helps prevent complications, reduces pain, and improves recovery time.
Understanding the diagnostic process empowers patients to communicate effectively with healthcare providers and make informed decisions about their care.
Treatment Options for a Pinched Nerve
Treating a pinched nerve depends on the severity, location, and underlying cause of the compression. Many cases improve with conservative, non-surgical approaches before medical intervention becomes necessary.
Home and lifestyle treatments are often the first step. Resting the affected area and avoiding movements that worsen symptoms can reduce pressure on the nerve. Applying ice or heat therapy may help relieve inflammation and soothe discomfort. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can reduce pain and swelling. Gentle stretching exercises and posture correction can also alleviate pressure, especially for nerves affected by poor ergonomics or repetitive strain.
Medical treatments may be recommended if symptoms persist. Physical therapy focuses on strengthening muscles, improving flexibility, and correcting posture to relieve nerve compression. In some cases, doctors may prescribe muscle relaxants or anti-inflammatory medications. For more severe nerve irritation, corticosteroid injections can reduce inflammation around the nerve, providing temporary or long-term relief.
Surgical intervention is considered only when conservative methods fail or if there is significant nerve damage or weakness. Surgical procedures vary depending on the nerve affected but often involve removing pressure from the nerve by correcting a herniated disc, removing bone spurs, or enlarging narrow nerve passages.
Recovery time depends on the cause and severity of the nerve compression, ranging from a few weeks for mild cases to several months for chronic or surgically treated conditions. Early diagnosis and proper treatment are key to reducing pain, restoring function, and preventing long-term nerve damage.
Can You Prevent a Pinched Nerve?
While not all pinched nerves can be completely avoided, many cases can be prevented by adopting healthy habits, proper posture, and safe movement practices. Prevention focuses on reducing pressure on nerves, maintaining flexibility, and strengthening supporting muscles.
Posture improvement is one of the most effective strategies. Sitting or standing with a straight back, shoulders relaxed, and head aligned over the spine reduces strain on neck and back nerves. When sitting for long periods, use an ergonomic chair, keep feet flat on the floor, and take short breaks to stand or stretch.
Exercise and stretching are crucial for nerve health. Regular physical activity strengthens core and back muscles, improving spinal support and reducing the likelihood of nerve compression. Stretching tight muscles, particularly in the neck, shoulders, and legs, helps relieve pressure that may irritate nerves. Yoga or pilates can be especially beneficial.
Weight management also plays a role. Excess body weight increases strain on the spine and joints, which can lead to nerve compression over time. Maintaining a healthy weight reduces this pressure.
Safe lifting techniques prevent sudden nerve injuries. When lifting heavy objects, bend at the knees, keep the back straight, and avoid twisting the spine. Repetitive motions or prolonged pressure on specific body parts, such as resting elbows on hard surfaces, should be minimized.
Finally, staying mindful of daily habits like avoiding cradling a phone between the shoulder and ear or keeping wrists straight during typing can prevent repetitive stress injuries that contribute to pinched nerves. By incorporating these preventative measures, many individuals can reduce the risk of nerve compression and maintain long-term mobility and comfort.
Frequently Asked Questions (FAQs About Pinched Nerves)
1. What does a pinched nerve feel like at first?
Early symptoms often include mild tingling, numbness, or a slight burning sensation. Pain may come and go and often worsens with certain movements or positions. Recognizing these early signs can help prevent worsening nerve compression.
2. Can a pinched nerve heal on its own?
Yes, many mild pinched nerves improve without medical intervention. Rest, posture correction, and gentle stretches often relieve pressure on the nerve. Recovery typically occurs within a few days to weeks, but severe cases may require professional treatment.
3. Is a pinched nerve dangerous?
Most pinched nerves are not life-threatening, but prolonged compression can cause permanent nerve damage. Seek medical attention if you experience severe pain, progressive weakness, loss of sensation, or bladder/bowel issues.
4. How do you know if nerve pain is getting worse?
Signs of worsening include increased intensity or frequency of pain, spreading tingling or numbness, muscle weakness, or difficulty performing daily tasks. Persistent symptoms should prompt a healthcare evaluation.
5. Can stress cause a pinched nerve?
Indirectly, yes. Stress can lead to muscle tension, poor posture, or repetitive movements, all of which increase pressure on nerves. Managing stress through exercise, relaxation techniques, and proper ergonomics can reduce risk.
6. How long does a pinched nerve last?
Mild cases may resolve in days or weeks. Moderate cases can last several weeks, and severe or untreated cases may persist for months or longer. Recovery depends on severity, underlying causes, and treatment.
7. What are common treatment options?
Treatments range from rest, ice or heat therapy, over-the-counter pain relief, and stretching to physical therapy, medications, corticosteroid injections, and, in severe cases, surgery. Early intervention improves recovery and reduces complications.
Conclusion
A pinched nerve can be uncomfortable, alarming, and disruptive to daily life, but understanding its symptoms, causes, and treatment options can help you manage it effectively.
The sensations associated with a pinched nerve sharp pain, burning, tingling, numbness, or muscle weakness often differ from ordinary muscle pain and can radiate along the affected nerve. Recognizing these signs early is key to preventing complications and promoting faster recovery.
Pinched nerves can occur in various parts of the body, including the neck, shoulders, arms, hands, lower back, legs, and feet.
Common causes include poor posture, repetitive movements, injuries, herniated discs, arthritis, or prolonged pressure on a nerve. While many mild cases improve with rest, stretching, and lifestyle adjustments, moderate to severe cases may require medical evaluation, physical therapy, or even surgical intervention.
Prevention plays an essential role in maintaining nerve health. Good posture, ergonomic workspaces, regular exercise, stretching, safe lifting techniques, and weight management can significantly reduce the risk of nerve compression.
Ultimately, paying attention to your body’s signals and addressing symptoms promptly can prevent long-term damage and improve your quality of life.
If you experience persistent pain, weakness, or numbness, consulting a healthcare professional ensures proper diagnosis, treatment, and relief. By staying informed and proactive, you can manage a pinched nerve effectively and maintain mobility and comfort.

Jordon Fox is an emerging artist and creative from Philadelphia, Pennsylvania, known for blending music, fashion, and fitness into his personal brand and artistic identity. He’s built a reputation as a multi-talented creator with a strong focus on authenticity and inspiring others.