If you’ve ever felt your heart suddenly start fluttering, racing, or beating irregularly, it can be a frightening experience.
Many people who search “what does AFib feel like” are trying to understand unusual sensations in their chest and whether they could signal something serious.
AFib, short for atrial fibrillation, is a common heart rhythm disorder that affects millions of people worldwide. But the way it feels can vary from person to person.
Some describe it as a rapid, chaotic heartbeat that seems out of sync.
Others notice skipped beats, pounding in the chest, shortness of breath, or sudden fatigue. And surprisingly, some people feel no symptoms at all.
Understanding what AFib feels like and how it differs from anxiety or other heart conditions can help you recognize warning signs and know when to seek medical attention.
In this guide, we’ll break it down clearly and calmly.
What Is AFib? Understanding the Basics
Atrial fibrillation, commonly called AFib, is a type of irregular heart rhythm, or arrhythmia, that originates in the heart’s upper chambers, known as the atria. Normally, your heart beats in a steady, coordinated rhythm, with electrical signals traveling in an orderly way to make your heart pump blood efficiently. In AFib, these electrical signals become chaotic, causing the atria to quiver or “fibrillate” instead of contracting properly.
This irregular activity leads to a heartbeat that can feel fast, erratic, or out of sync with the rest of your body. Blood may not flow as efficiently through the heart, increasing the risk of clots forming and potentially causing a stroke.
AFib can be intermittent, with episodes that start and stop suddenly, or persistent, lasting for longer periods and sometimes requiring medical treatment. Some people experience it briefly and barely notice it, while others may feel significant symptoms that disrupt daily life.
Understanding what AFib is helps make sense of why it produces such a wide range of sensations from subtle fluttering to severe racing or pounding in the chest. It also explains why some people may feel shortness of breath, dizziness, or fatigue during an episode. By recognizing the basic mechanics of AFib, you’ll be better prepared to identify its symptoms and respond appropriately.
What Does AFib Feel Like?
AFib symptoms can vary widely from person to person, making it a confusing condition to recognize. The most commonly reported sensation is a fluttering or quivering feeling in the chest, sometimes described as if the heart is “skipping” or “flopping.” Many people also notice a rapid or pounding heartbeat, which can feel out of sync with their normal rhythm.
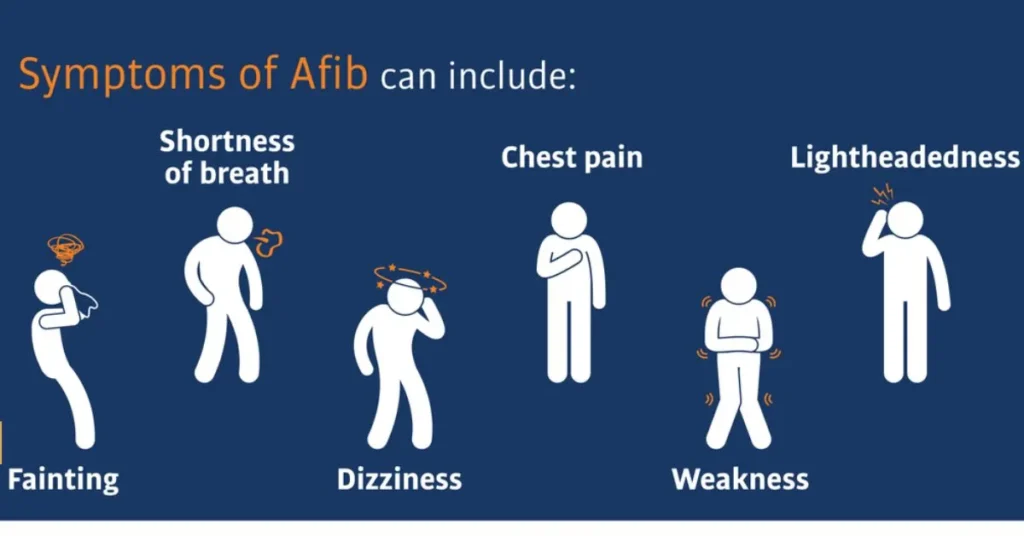
Some individuals feel skipped or extra beats, while others experience a more continuous, chaotic racing sensation. These irregular rhythms may appear suddenly and unexpectedly, often catching people off guard. Physical symptoms can also extend beyond the chest. Shortness of breath, dizziness, lightheadedness, fatigue, or weakness are common, particularly during longer AFib episodes. Some people may even feel pressure or discomfort in the chest, though severe pain is less common and could indicate another heart problem.
Interestingly, AFib doesn’t always produce noticeable symptoms. This is called silent AFib, and it can go undetected for years, increasing the risk of stroke without the person realizing anything is wrong.
The emotional impact of AFib shouldn’t be overlooked. Experiencing sudden irregular heartbeats can provoke anxiety, fear, or panic, which can sometimes make the physical sensations feel even more intense.
Understanding these symptoms is crucial because recognizing AFib early allows for prompt medical evaluation, treatment, and lifestyle adjustments to reduce complications and improve overall heart health.
What an AFib Episode Feels Like
AFib episodes, also called “flares” or “attacks,” can feel very different depending on their duration, intensity, and the individual experiencing them. Some episodes begin suddenly, with the heart racing or fluttering without warning. Others develop gradually, starting as subtle irregular beats that slowly increase in intensity.
The length of an episode can vary widely. Short episodes may last just a few minutes, leaving a brief fluttering sensation or a feeling that your heartbeat “skipped a beat.” Longer episodes can persist for hours or even days, often accompanied by fatigue, shortness of breath, and a constant awareness of the irregular heartbeat. In persistent AFib, the episode may not stop on its own, and medical intervention could be necessary to restore a normal rhythm.
During an episode, people often describe sensations that are difficult to ignore. Some compare it to “a fish flopping in the chest”, while others say it feels like the heart is “trying to catch up” or “beating out of sync with the body.” Episodes can also trigger dizziness, lightheadedness, or even a faint feeling, especially if the heart is beating very rapidly.
The unpredictability of AFib episodes can cause anxiety or stress, which may make the sensations feel even more pronounced. Keeping track of the timing, duration, and triggers of episodes can be valuable information for doctors, helping them diagnose the type of AFib and determine the most effective treatment plan.
AFib vs Anxiety or Panic Attack
Many people confuse the sensations of AFib with anxiety or a panic attack because both can cause a racing heart, shortness of breath, and chest discomfort. However, there are key differences that can help you distinguish between the two.
Heart rhythm: AFib produces an irregular and often chaotic heartbeat, whereas anxiety or panic attacks usually cause a rapid but regular heartbeat. You might notice your pulse skipping or pounding unpredictably during AFib, while anxiety tends to feel like your heart is simply racing.
Duration: Panic attacks generally peak within 10–20 minutes and then gradually subside. AFib episodes can last minutes, hours, or even days, sometimes stopping and starting unpredictably.
Triggers: Anxiety-related heart racing is often tied to stressful situations, worry, or fear, while AFib can occur without an obvious trigger, although stress, alcohol, or stimulants may worsen it.
Other symptoms: Panic attacks frequently involve feelings of intense fear, sweating, trembling, or a sense of impending doom. AFib, on the other hand, can bring fatigue, dizziness, shortness of breath, or chest discomfort without necessarily causing panic.
Why it matters: Misinterpreting AFib for anxiety can delay diagnosis and treatment, increasing the risk of complications like stroke or heart failure. If you experience irregular heartbeats, skipped beats, or prolonged episodes, it’s important to seek medical evaluation, even if you suspect anxiety.
Understanding these differences can help you respond appropriately and give doctors accurate information, which is essential for safe and effective management of your heart health.
When Is AFib Dangerous?
While some people experience mild AFib episodes that cause little discomfort, it’s important to understand that AFib can be serious if left untreated. One of the most significant risks is stroke. Because the atria are quivering instead of contracting normally, blood can pool in the heart, increasing the chance of forming blood clots. If a clot travels to the brain, it can cause a stroke, which may result in long-term disability or even death.
Another concern is heart failure. AFib can reduce the heart’s efficiency, especially during rapid or prolonged episodes, making it harder for your body to get the oxygen it needs. Over time, this can weaken the heart and lead to chronic heart problems.
Certain symptoms indicate that AFib may require immediate medical attention. Seek emergency care if you experience:
- Severe chest pain or pressure
- Fainting or near-fainting
- Sudden shortness of breath
- Signs of a stroke, including facial drooping, arm weakness, or difficulty speaking
Even if symptoms seem mild, repeated or prolonged AFib episodes still carry long-term health risks, including increased strain on the heart and elevated stroke risk.
Recognizing when AFib is dangerous is key to preventing complications. Early medical evaluation and treatment, such as medications, lifestyle adjustments, or procedures like cardioversion, can help control the heart rhythm, reduce symptoms, and protect your overall health. Being proactive about AFib symptoms can make a significant difference in long-term outcomes.
How Doctors Diagnose AFib
If you experience irregular heartbeats, skipped beats, or other symptoms that suggest AFib, a doctor will perform a thorough evaluation to confirm the diagnosis and determine the best treatment. Diagnosis usually begins with a physical exam, during which a doctor listens to your heart and checks your pulse for irregularities.
The most common and essential test is an electrocardiogram (ECG or EKG). This painless test records the electrical activity of your heart and can reveal whether the atria are beating irregularly. An ECG is often the first step in diagnosing AFib, especially if the episode is occurring during the visit.
For patients whose episodes are intermittent, doctors may recommend Holter monitoring, which involves wearing a small portable device for 24–48 hours to track heart rhythm continuously. For longer-term tracking, an event monitor can be worn for weeks or even months, allowing the patient to record episodes as they happen.
Additional tests may include a transthoracic echocardiogram, which uses ultrasound to visualize the heart’s structure and function, and blood tests to check for underlying conditions like thyroid disorders or electrolyte imbalances that could trigger AFib.
Accurate diagnosis is essential because it helps doctors classify the type of AFib paroxysmal, persistent, or permanent and determine the most effective treatment, whether that’s medication, lifestyle changes, or a procedure like cardioversion or ablation.
By understanding the diagnostic process, patients can feel more confident, provide accurate symptom details, and work closely with their healthcare team to manage AFib effectively.
Who Is Most at Risk for AFib
Atrial fibrillation can affect anyone, but certain groups of people are more likely to develop it. Age is one of the most significant risk factors AFib becomes more common after age 60, and the likelihood increases with each decade of life.
Heart-related conditions also play a major role. People with high blood pressure, coronary artery disease, heart valve problems, or a history of heart attacks are at higher risk. Structural changes in the heart, such as enlarged atria, can disrupt normal electrical signals and trigger AFib.
Other medical conditions increase susceptibility, including diabetes, thyroid disorders, obesity, and sleep apnea. Lifestyle factors can also contribute: heavy alcohol use, excessive caffeine, and chronic stress may provoke AFib episodes in some individuals.
Family history is another important factor. If a close relative has had AFib, your risk may be higher due to genetic predispositions affecting heart rhythm and structure.
Men tend to develop AFib slightly more often than women, but women with AFib may have a higher risk of complications such as stroke.
Understanding who is at risk helps both patients and doctors monitor for early signs, manage underlying conditions, and take preventive measures. Regular checkups, maintaining a healthy weight, controlling blood pressure, limiting alcohol, and managing chronic illnesses can all reduce the risk of developing AFib or help manage it more effectively.
What To Do If You Notice Symptoms
If you experience symptoms that could indicate AFib, such as fluttering, racing, or irregular heartbeats, it’s important to take action promptly. The first step is to stay calm. Anxiety can intensify the sensation of an irregular heartbeat, making symptoms feel worse.
Next, check your pulse. You may notice an irregular or unusually fast heartbeat, which can help you describe your experience accurately to a healthcare professional. Sit or lie down if you feel dizzy, lightheaded, or weak, and try to remain still while your body adjusts.
Avoid stimulants such as caffeine or energy drinks, which can exacerbate symptoms. Keep a record of your episodes, noting the time, duration, intensity, and any triggers like stress, alcohol, or exercise. This information is extremely helpful for doctors when diagnosing AFib and creating a treatment plan.
It’s crucial to seek medical evaluation, even if the symptoms are mild or intermittent. A healthcare professional can perform tests such as an ECG, Holter monitor, or echocardiogram to confirm whether AFib is present and determine the type.
Seek emergency care immediately if you experience severe chest pain, fainting, extreme shortness of breath, or signs of stroke such as facial drooping, arm weakness, or difficulty speaking.
Early recognition and action can reduce the risk of complications such as stroke, heart failure, or prolonged episodes. By responding promptly and working closely with your doctor, you can manage AFib effectively and maintain heart health.
Treatment Options for AFib
Managing atrial fibrillation effectively involves a combination of medications, procedures, and lifestyle changes tailored to each individual. The primary goals are to control the heart rate, maintain a normal rhythm, and reduce the risk of stroke.
Medications are often the first line of treatment. Rate control drugs help slow a rapid heartbeat, while rhythm control medications aim to restore and maintain a regular heart rhythm. Doctors may also prescribe anticoagulants, or blood thinners, to prevent blood clots and reduce stroke risk.
For patients whose AFib episodes are frequent, persistent, or severe, procedures may be recommended. Cardioversion involves delivering a controlled electric shock to the heart to restore a normal rhythm. Catheter ablation is another option, in which doctors destroy small areas of heart tissue causing the abnormal signals, reducing or eliminating AFib episodes.
Lifestyle changes play a critical role in managing AFib and preventing flare-ups. Maintaining a healthy weight, managing stress, limiting alcohol and caffeine, exercising regularly, and controlling underlying conditions such as high blood pressure or diabetes can make a significant difference.
In some cases, a combination of these treatments is necessary to achieve optimal results. Regular follow-up appointments are important to monitor the heart rhythm, adjust medications, and evaluate the effectiveness of interventions.
By understanding the available treatment options, patients can work with their doctors to create a personalized plan that reduces symptoms, prevents complications, and improves quality of life while living with AFib.
Living With AFib
Living with atrial fibrillation requires awareness, routine monitoring, and lifestyle adjustments to reduce symptoms and prevent complications. One of the most important steps is tracking your symptoms. Keep a log of episodes, noting the time, duration, intensity, and any potential triggers. This information helps your doctor adjust treatments and better understand your AFib patterns.
Lifestyle choices play a significant role in managing AFib. Regular exercise, tailored to your doctor’s recommendations, can strengthen the heart and improve overall cardiovascular health. Avoiding excessive alcohol, caffeine, and stimulants helps prevent episodes from being triggered. Managing stress through meditation, yoga, or relaxation techniques can also reduce flare-ups.
Dietary habits matter too. Eating a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins supports cardiovascular function. Controlling weight, blood pressure, and blood sugar levels is essential, as obesity, hypertension, and diabetes are risk factors for AFib.
Regular medical check-ups and routine monitoring are critical. Your doctor may recommend periodic ECGs, Holter monitoring, or blood tests to ensure treatments are effective and to detect any new concerns early.
Finally, education and support are key. Understanding your condition, knowing warning signs, and seeking support from healthcare professionals or AFib support groups can reduce anxiety and improve quality of life. By actively managing symptoms and following medical guidance, people with AFib can maintain a healthy, active lifestyle while minimizing the risks associated with the condition.
Frequently Asked Questions About AFib
1. Can AFib go away on its own?
Some people experience paroxysmal AFib, where episodes start and stop spontaneously. While short episodes may resolve on their own, repeated or prolonged AFib requires medical evaluation to prevent complications such as stroke or heart failure.
2. Does AFib always cause symptoms?
Not always. Many people have silent AFib, experiencing no noticeable symptoms. This is why regular checkups and pulse monitoring are important, especially if you have risk factors like high blood pressure, diabetes, or a family history of AFib.
3. How is AFib diagnosed?
Doctors use tools such as ECG/EKG, Holter monitors, event monitors, echocardiograms, and blood tests to detect abnormal heart rhythms and identify underlying causes. Keeping a symptom diary can help doctors capture intermittent episodes.
4. Can young people get AFib?
Yes, although AFib is more common in older adults, it can occur in younger people, especially if there are underlying heart conditions, thyroid problems, or lifestyle factors such as heavy alcohol use or high-intensity exercise.
5. Is AFib dangerous?
AFib increases the risk of stroke and heart failure. Prompt diagnosis, treatment, and lifestyle management significantly reduce complications and improve quality of life.
6. Can stress or anxiety trigger AFib?
Stress, anxiety, caffeine, or alcohol may trigger episodes in some individuals, but AFib is caused by irregular electrical signals in the heart. Stress management can help reduce episodes but does not replace medical treatment.
7. What should I do if I feel an AFib episode?
Check your pulse, rest, avoid stimulants, and seek medical evaluation, especially if the episode is prolonged, severe, or accompanied by chest pain, dizziness, or shortness of breath.
Final Thoughts
Experiencing an irregular or racing heartbeat can be unsettling, and understanding what AFib feels like is the first step toward managing it effectively.
Atrial fibrillation varies widely from person to person some people feel a fluttering, pounding, or skipped heartbeat, while others may experience shortness of breath, dizziness, fatigue, or even no symptoms at all.
Recognizing the signs early allows for timely medical evaluation and reduces the risk of serious complications such as stroke or heart failure.
AFib is a manageable condition with the right combination of medical care, lifestyle adjustments, and ongoing monitoring.
Medications, procedures, and preventive strategies tailored to each individual can help control heart rate, maintain a regular rhythm, and reduce stroke risk.
Lifestyle changes, including stress management, exercise, a heart-healthy diet, and avoiding triggers like alcohol or caffeine, also play an important role in minimizing episodes and improving overall well-being.
Regular checkups, symptom tracking, and communication with healthcare providers are essential.
Even if symptoms feel mild or intermittent, seeking evaluation ensures proper diagnosis and treatment.
Remember, AFib is common but serious, and knowledge is empowering.
By understanding your symptoms, knowing when to seek help, and following medical guidance, you can take control of your heart health, reduce anxiety, and live a safe, active life.

Jordon Fox is an emerging artist and creative from Philadelphia, Pennsylvania, known for blending music, fashion, and fitness into his personal brand and artistic identity. He’s built a reputation as a multi-talented creator with a strong focus on authenticity and inspiring others.