Searching for “what does anal cancer look like” is often driven by concern, uncertainty, or noticing unusual changes in the anal area. Anal cancer is relatively rare, but its early signs can closely resemble common and less serious conditions such as hemorrhoids, anal fissures, or skin irritation. Because of this, many people delay seeking medical advice, which can affect outcomes.
Understanding how anal cancer may appear—both visually and through physical symptoms—can help you recognize potential warning signs sooner.
This article provides clear, non graphic descriptions of what anal cancer can look like in its early and advanced stages, along with symptoms that often accompany these changes. While appearance alone cannot confirm a diagnosis, awareness is a powerful first step.
Early detection significantly improves treatment success, so knowing when something looks or feels abnormal—and when to consult a healthcare professional—can make a meaningful difference to your health and peace of mind.
What Is Anal Cancer? (Medical Overview)
Anal cancer is a type of cancer that develops in the tissues of the anus, which is the opening at the end of the digestive tract where stool leaves the body. Although it is less common than other gastrointestinal cancers, such as colorectal cancer, anal cancer is significant because its early symptoms are often subtle and easily mistaken for minor anal conditions. The most common type is squamous cell carcinoma, which begins in the thin, flat cells lining the anal canal. Less common types include adenocarcinoma, melanoma, and basal cell carcinoma, each of which may look and behave differently.
In many cases, anal cancer develops slowly over time, starting with abnormal cell changes that may not cause immediate discomfort. These abnormal cells can form small lesions, growths, or sores that gradually change in size, texture, or appearance. Infection with human papillomavirus (HPV) is one of the leading risk factors, as certain HPV strains can cause cellular changes that increase cancer risk. Other contributing factors include smoking, a weakened immune system, and chronic inflammation in the anal area.
Understanding what anal cancer is helps explain why its appearance can vary so much from person to person. Some tumors develop on the outer skin around the anus, making them more visible, while others grow inside the anal canal and are harder to see without a medical exam. Because of this variability, visual changes alone are not enough to diagnose anal cancer. However, learning how and where it develops provides important context for recognizing potential warning signs and seeking timely medical evaluation.
Anatomy of the Anal and Perianal Area
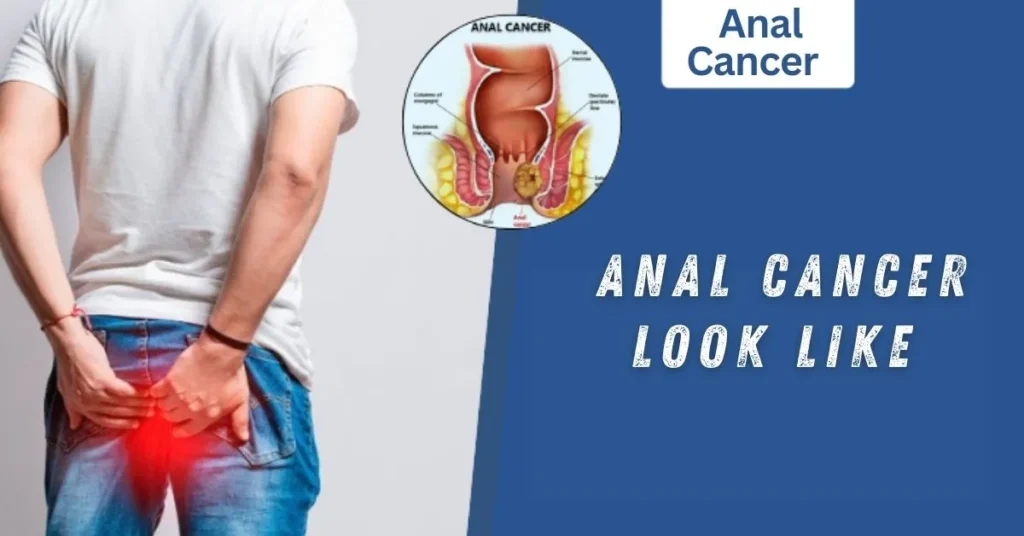
To understand what anal cancer looks like, it helps to first understand the basic anatomy of the anal and perianal area. The anus is the external opening at the end of the digestive tract, while the anal canal is the short passage just inside the body that connects the rectum to the outside. Surrounding the anus is the perianal skin, which is similar to regular skin elsewhere on the body. Anal cancer can develop in any of these areas, and its appearance often depends on its exact location.
Cancers that form on the perianal skin are more likely to be visible to the naked eye. These may appear as small lumps, raised patches, sores, or areas of skin that look discolored or thickened. Because this skin is exposed, changes are sometimes noticed earlier, especially during hygiene or self care routines. In contrast, tumors that develop inside the anal canal are not usually visible without medical tools. These internal cancers may cause symptoms such as bleeding, pain, or a sensation of pressure rather than obvious visual changes.
The anal area also contains many blood vessels and nerve endings, which is why even small abnormalities can lead to bleeding or discomfort. Additionally, the tight space of the anal canal means that any growth, even a small one, can interfere with bowel movements. Understanding this anatomy explains why anal cancer can look different from person to person and why some cases present mainly with visible skin changes, while others are detected because of symptoms rather than appearance.
What Does Anal Cancer Look Like in Early Stages?
In its early stages, anal cancer often causes subtle changes that can be easy to overlook or mistake for harmless conditions. Early anal cancer may appear as a small lump, bump, or nodule near or inside the anus. These growths are often firm and may not be painful at first, which is why many people do not seek medical attention right away. In some cases, the skin around the anus may look slightly red, irritated, or discolored, without obvious swelling.
Another early sign can be a flat or slightly raised lesion that feels rough or thickened compared to the surrounding skin. These changes may resemble hemorrhoids, ingrown hairs, or minor skin infections. Some people notice light bleeding, spotting on toilet paper, or mucus like discharge, especially after bowel movements. Because bleeding is commonly associated with hemorrhoids, it is frequently ignored.
Itching or mild discomfort can also occur in the early stages, though these symptoms are not always present. Importantly, early anal cancer does not always cause significant pain. The absence of severe symptoms often leads to delays in diagnosis. Changes may remain stable for weeks or slowly worsen over time, rather than resolving on their own.
What makes early anal cancer particularly challenging is that it often does not heal like benign conditions. While hemorrhoids or minor tears tend to improve with treatment or time, cancer related changes usually persist or gradually worsen. Any anal lump, sore, or bleeding that lasts longer than two to three weeks, or that continues to return, should be evaluated by a healthcare professional. Recognizing these early visual and physical clues can play a critical role in detecting anal cancer at a more treatable stage.
Visual Signs of Anal Cancer (Descriptive, Non Graphic)
As anal cancer progresses, the visual signs often become more noticeable, especially when the cancer affects the outer anal or perianal skin. One of the most common visible signs is a persistent sore or ulcer near the anus that does not heal. Unlike minor cuts or irritation, these sores may remain open, slowly enlarge, or develop an irregular shape over time. The surrounding skin may appear inflamed or unusually firm to the touch.
Anal cancer can also present as a hard or irregular growth. These growths may be raised above the skin surface or felt just beneath it. They are often different in texture from hemorrhoids, which tend to feel softer. In some cases, the affected area may look thickened, scaly, or rough, similar to a chronic skin condition that does not respond to typical treatments.
Changes in skin color are another possible sign. The skin around the anus may become reddish, darker, or paler than normal. Swelling or puffiness around the anal opening can occur, sometimes causing the area to look distorted or asymmetrical. Some people also notice unusual discharge, such as mucus or fluid, which may stain underwear.
It is important to note that these visual changes are not always dramatic. Anal cancer does not have a single, distinct appearance, and the signs can vary depending on the cancer type and location. Because many of these changes resemble noncancerous conditions, they are often misinterpreted. Any visible anal abnormality that persists, changes in appearance, or worsens over time should be medically evaluated to rule out serious causes and ensure timely diagnosis.
What Does Advanced Anal Cancer Look Like?
In more advanced stages, anal cancer tends to cause clearer and more severe visual and physical changes. Tumors may grow larger and become more obvious around the anal opening or within the anal canal. Externally, advanced anal cancer can appear as a large, irregular mass that may protrude or distort the normal shape of the anus. These growths often have uneven borders and may feel very firm or hard to the touch.
Non healing open sores or ulcers are more common at this stage and may be accompanied by ongoing inflammation. The skin around the affected area can look severely swollen, irritated, or broken down. Persistent bleeding is another key sign, which may occur even without bowel movements. Some people notice blood in their stool, on toilet paper, or in their underwear.
Advanced anal cancer is also more likely to cause significant pain, especially during sitting or bowel movements. The pain may be constant or worsen over time. As the tumor grows, it can partially block the anal canal, leading to changes in bowel habits such as difficulty passing stool, a feeling of incomplete emptying, or unusually narrow stools.
In some cases, the cancer may spread to nearby lymph nodes, causing visible or palpable swelling in the groin area. Unusual discharge with a strong odor may also occur due to tissue damage or infection. These advanced signs indicate a serious condition that requires immediate medical attention. While advanced anal cancer is more challenging to treat, recognizing these symptoms promptly can still improve outcomes and guide appropriate treatment options.
Physical Sensations That Accompany the Appearance
Along with visible changes, anal cancer often causes physical sensations that can alert someone that something is wrong. One of the most common sensations is persistent pain or discomfort in or around the anus. This pain may start as mild pressure and gradually become more intense, especially during bowel movements or while sitting for long periods. Unlike temporary irritation, this discomfort tends to worsen rather than improve over time.
Itching or burning around the anal area is another frequent complaint. While itching is common with conditions like hemorrhoids or skin irritation, cancer related itching often persists despite good hygiene or over the counter treatments. Some people experience a constant sensation of fullness, as if there is something stuck in the anal canal, even after a bowel movement.
As anal cancer progresses, bowel movements may become increasingly uncomfortable. Pain during defecation can lead to straining, which may further aggravate symptoms. In some cases, individuals notice changes in stool shape, such as stools becoming narrower, due to partial blockage of the anal canal. Bleeding may accompany these sensations, adding to discomfort and concern.
Another important physical sign is tenderness or swelling in nearby areas, particularly the groin. This can happen when cancer spreads to nearby lymph nodes. Some people also report fatigue or a general feeling of being unwell, especially in later stages.
These physical sensations are significant because they often persist and gradually intensify. Any ongoing anal pain, pressure, itching, or unusual sensations that last longer than a few weeks should not be ignored. When combined with visible changes, they strongly signal the need for a professional medical evaluation.
Anal Cancer Symptoms Beyond Appearance
While visual signs and physical sensations are important, anal cancer often produces symptoms that go beyond what you can see. One of the most common and early symptoms is rectal bleeding. This can range from light spotting to more noticeable blood in the stool or on toilet paper. Because bleeding is also common with hemorrhoids, fissures, or infections, it is often dismissed or attributed to minor issues. However, persistent or unexplained bleeding should always be evaluated.
Changes in bowel habits are another symptom. People may notice narrower stools, increased frequency, constipation, or a feeling that the bowel does not empty completely. Some may experience difficulty passing stool due to tumor growth partially blocking the anal canal. Pain during bowel movements or a persistent sense of pressure can accompany these changes.
Anal cancer can also cause anal discharge, which may be mucus-like or slightly bloody. In some cases, an unpleasant odor may develop if tissue damage or infection occurs. Other systemic symptoms can appear, especially in advanced stages. These include fatigue, unexplained weight loss, and swollen lymph nodes, typically in the groin area.
It is important to understand that not all symptoms appear at once. Early anal cancer may present only with mild bleeding or a small lump, while later stages combine multiple signs, making them harder to ignore. Awareness of these non-visual symptoms is critical because anal cancer can sometimes progress internally before producing obvious external signs. Paying attention to persistent or unusual changes in the anal area, bowel habits, or overall well-being can lead to earlier detection and significantly improve treatment outcomes.
Anal Cancer vs Hemorrhoids, Fissures, and Warts
Anal cancer is often confused with other common anal conditions, such as hemorrhoids, anal fissures, or warts, because some symptoms overlap. However, there are key differences that can help distinguish them.
Anal Cancer vs Hemorrhoids: Hemorrhoids are swollen blood vessels in the anal area and are usually soft, tender, and sometimes painful during bowel movements. They may bleed occasionally but often improve with home treatments, such as fiber, hydration, or topical ointments. Anal cancer lumps, in contrast, are typically firmer, irregular, and do not resolve with standard hemorrhoid care. Persistent bleeding, growths that do not shrink, or sores that last longer than a few weeks are more concerning.
Anal Cancer vs Anal Fissures: Anal fissures are small tears in the lining of the anus, often caused by constipation or hard stools. They cause sharp pain during bowel movements and minor bleeding. Unlike fissures, cancer-related lesions persist over time and may increase in size, sometimes without causing immediate pain.
Anal Cancer vs Anal Warts: Anal warts, caused by HPV infection, appear as small, soft, cauliflower-like growths around the anus. They are usually painless but may be itchy. Anal cancer growths are harder, irregular, and often accompanied by bleeding, sores, or persistent discomfort, setting them apart from warts.
Because the appearance of anal cancer can mimic these benign conditions, self-diagnosis is unreliable. Any lump, sore, or abnormal growth that does not improve or continues to worsen should be evaluated by a healthcare professional. Early distinction between benign and potentially malignant changes is critical for timely treatment and better outcomes.
If you want, I can next write the section “Does Anal Cancer Always Look the Same?” with 250 words. Do you want me to continue?
Does Anal Cancer Always Look the Same?
Anal cancer does not have a single, uniform appearance, which can make early detection challenging. Its visual presentation varies depending on factors such as the cancer type, its location, the stage of growth, and individual differences in skin tone or tissue structure. Some tumors develop on the external perianal skin, where they may appear as visible lumps, sores, or patches of discolored or thickened skin. Others grow inside the anal canal, making them difficult to see without medical examination, and they may primarily cause internal symptoms like bleeding, a sense of fullness, or pain.
The type of anal cancer also influences its appearance. Squamous cell carcinoma, the most common type, often forms firm nodules or ulcerated patches. Adenocarcinoma may develop higher inside the anal canal and produce fewer visible signs until later stages. Rare types like melanoma or basal cell carcinoma may appear as darkly pigmented spots or unusual skin lesions.
Skin tone and individual anatomy further contribute to variability. For example, redness may be more noticeable on lighter skin, while discoloration may be subtler on darker skin. Some people may experience multiple small growths, while others may have a single lesion.
Because of this variability, appearance alone is insufficient for diagnosis. Persistent changes in the anal area, whether subtle or more obvious, should always be evaluated by a healthcare professional. Understanding that anal cancer can look very different from person to person emphasizes the importance of monitoring any unusual or persistent changes and seeking timely medical assessment for early detection and treatment.
What Causes These Visual Changes?
The visual changes seen in anal cancer are the result of abnormal cellular growth and tissue disruption. Anal cancer begins when healthy cells in the lining of the anus undergo mutations that cause them to grow uncontrollably. Over time, these abnormal cells can form lumps, sores, or thickened patches of skin. Unlike normal tissue, cancerous tissue may not heal properly, which is why lesions and ulcers associated with anal cancer often persist or worsen.
Human papillomavirus (HPV) infection is a major contributor to these cellular changes. Certain high-risk strains of HPV can cause the anal cells to mutate, increasing the likelihood of cancer development. HPV-related lesions can initially appear as small warts, but in some cases, persistent infection leads to the formation of cancerous growths.
Other factors can accelerate these visual changes. Chronic inflammation in the anal area, whether from infections, long-standing hemorrhoids, or repeated irritation, can make the tissue more susceptible to abnormal growth. Smoking is another significant risk factor, as it weakens the immune system and impairs the body’s ability to repair damaged cells. A weakened immune system, including conditions like HIV/AIDS, also increases susceptibility to the cellular changes that lead to anal cancer.
The location of the tumor—whether on the external perianal skin or inside the anal canal—affects how these changes present visually. External tumors may appear as lumps, sores, or thickened patches, while internal tumors often cause subtle symptoms like bleeding or fullness before visible signs appear. Recognizing these underlying causes helps explain why anal cancer can manifest in various ways, reinforcing the need for careful observation and timely medical evaluation of any persistent anal changes.
Who Is at Higher Risk of Anal Cancer?
Certain individuals are more likely to develop anal cancer due to factors that affect cellular health, immunity, and exposure to risk-causing agents. Human papillomavirus (HPV) infection is the most significant risk factor. HPV, particularly high-risk strains like HPV 16 and 18, can trigger mutations in anal cells that may eventually lead to cancer. People with persistent or long-term HPV infections are therefore at higher risk.
Smoking is another major contributor. Tobacco use weakens the immune system, damages DNA, and impairs the body’s natural ability to repair abnormal cells. Studies show that smokers are more likely to develop anal cancer than non-smokers.
Individuals with a weakened immune system, such as those living with HIV/AIDS or who are on immunosuppressive medications, also face higher risk. The immune system plays a key role in detecting and destroying abnormal cells before they become cancerous, so reduced immune function allows these cells to grow unchecked.
Age and gender play a role as well. Anal cancer is more commonly diagnosed in adults over 50, though younger adults can also be affected, particularly if they have risk factors like HPV infection. Women are slightly more likely than men to develop anal cancer, often due to HPV-related cellular changes.
Other risk factors include chronic anal irritation or inflammation, history of anal warts, or previous cancers in the genital or rectal region. Understanding these risk factors is crucial because individuals who fall into one or more high-risk categories should monitor for changes in the anal area and consider regular medical screenings. Early detection is especially important for high-risk populations, as it can greatly improve treatment success and overall prognosis.
When Should You Be Concerned?
Recognizing when to seek medical attention is critical, as early detection of anal cancer significantly improves treatment outcomes. While many anal conditions are harmless, there are specific signs and changes that should not be ignored. One of the most important red flags is persistent anal bleeding. Light spotting may seem minor, but if it continues for more than two to three weeks or occurs without an obvious cause, it warrants evaluation by a healthcare professional.
Lumps, growths, or sores that do not heal are another concern. Unlike hemorrhoids or minor skin irritations, cancer-related lumps often remain firm, irregular, or progressively enlarge over time. Any sore that persists, especially if accompanied by changes in skin color, texture, or thickness, should be checked promptly.
Pain or discomfort that worsens over time, especially during sitting or bowel movements, is also significant. While occasional anal discomfort can result from minor issues, persistent or intensifying pain may indicate an underlying problem. Changes in bowel habits, such as narrower stools, a sense of blockage, or incomplete evacuation, are additional warning signs.
Other symptoms that require attention include unusual discharge, foul-smelling fluid, swelling in the groin, or systemic signs like unexplained fatigue or weight loss. Importantly, even if visual changes are subtle or internal, these physical signs can signal that something is wrong.
The general rule is simple: any persistent, unusual, or worsening anal symptom should be evaluated by a healthcare professional. Early consultation allows for timely diagnosis, which can dramatically improve prognosis. Being proactive rather than waiting for symptoms to resolve on their own is essential for maintaining anal and overall health.
How Doctors Examine and Diagnose Anal Cancer
When anal cancer is suspected, a healthcare professional will perform a series of examinations and tests to confirm the diagnosis. The evaluation usually begins with a physical examination of the anal and perianal area. The doctor will look for visible lumps, sores, discoloration, or thickened skin, and may gently feel for irregularities around the anus. Even subtle changes can provide important clues.
A digital rectal exam (DRE) is often performed next. During this procedure, the doctor inserts a gloved, lubricated finger into the anal canal to feel for internal lumps, nodules, or areas of abnormal tissue that may not be visible externally. This simple exam is a key first step in detecting internal tumors.
If an abnormality is found, an anoscopy or high-resolution anoscopy (HRA) may be recommended. This procedure uses a small scope with a light to closely examine the anal canal and rectum, helping the doctor identify suspicious lesions. Any abnormal areas discovered during this exam are typically biopsied.
A biopsy is the definitive test for diagnosing anal cancer. A small sample of tissue is removed and examined under a microscope for cancerous cells. The biopsy also helps determine the type of anal cancer, which is essential for planning treatment.
In some cases, imaging tests such as MRI, CT scans, or PET scans are used to assess the extent of the tumor and whether it has spread to nearby lymph nodes or other tissues.
It is important to remember that a proper diagnosis combines visual assessment, physical examination, and microscopic confirmation. Self-diagnosis is unreliable because early anal cancer can resemble benign conditions. Consulting a healthcare professional ensures accurate detection, timely treatment, and better outcomes.
Can You See Anal Cancer Yourself?
Many people wonder whether they can detect anal cancer on their own. The answer is sometimes, but not always, because the visibility of anal cancer depends on its location and stage. Tumors that develop on the perianal skin, the outer area around the anus, may be noticeable as lumps, sores, or patches of discolored or thickened skin. In such cases, careful self-observation during hygiene routines or while using a mirror may help identify unusual changes early.
However, not all anal cancers are visible externally. Tumors inside the anal canal may grow without producing obvious visual signs. Early-stage internal cancers often cause subtle symptoms such as light bleeding, a feeling of fullness, or mild discomfort, rather than visible lumps. Because of this, relying solely on self-checks can result in delayed detection.
Even when a growth is visible externally, it can be difficult to distinguish between benign conditions like hemorrhoids, warts, or minor skin irritation and actual cancer. Persistent, unusual changes that do not improve with standard care are the most concerning. Features such as firmness, irregular shape, non-healing sores, or worsening discoloration are more suspicious than temporary irritation.
Self-examination can be a useful first step, but it is not a replacement for professional evaluation. Any persistent or unusual changes in the anal area should be assessed by a healthcare provider. Early medical consultation allows for diagnostic procedures like anoscopy or biopsy, which are necessary to confirm whether the changes are due to cancer. Monitoring symptoms while seeking timely medical care is the safest way to detect anal cancer early.
Emotional Impact of Noticing Anal Changes
Noticing unusual changes in the anal area can be a source of stress, embarrassment, and anxiety for many people. Because the anus is a private and often stigmatized part of the body, individuals may feel uncomfortable discussing symptoms with friends, family, or even healthcare professionals. This emotional barrier can lead to delays in seeking medical care, which in turn may allow cancer or other serious conditions to progress.
Fear is a common response. Many people worry that a lump, sore, or bleeding could be cancer, and the uncertainty can cause significant emotional strain. This anxiety can be compounded by the stigma surrounding anal health and sexual health, making individuals hesitant to mention symptoms during routine checkups. Feeling isolated or ashamed may prevent someone from taking timely action, even when early intervention could greatly improve outcomes.
On the other hand, acknowledging and addressing these changes proactively can provide peace of mind. Seeking medical evaluation allows for accurate diagnosis and can relieve the fear of the unknown. Understanding that early detection makes treatment more effective empowers individuals to act despite embarrassment or discomfort.
Support is also important. Talking to a trusted healthcare provider, counselor, or patient support group can help reduce anxiety and provide guidance. Many people find reassurance in knowing they are not alone and that professional care exists for managing and treating anal conditions.
Ultimately, the emotional impact of noticing anal changes highlights the importance of overcoming stigma and fear. Prompt attention to unusual symptoms, combined with emotional support, ensures both physical and mental well-being, while maximizing the chances of early and successful treatment.
Treatment Overview and How Appearance Changes After Treatment
Once anal cancer is diagnosed, treatment typically involves one or more approaches depending on the cancer’s type, size, and stage. Surgery is often used to remove tumors that are localized and accessible. After surgical removal, the appearance of the anal area may change, sometimes resulting in scars, small depressions, or slightly altered skin texture. In some cases, larger surgeries may affect the shape or function of the anus, requiring additional care during healing.
Radiation therapy is another common treatment, often combined with chemotherapy. Radiation can cause temporary changes to the skin around the anus, including redness, swelling, dryness, or irritation. These effects are generally temporary, and the skin usually heals over weeks to months, though it may remain slightly sensitive or discolored in some individuals.
Chemotherapy targets cancer cells systemically and may not visibly change the anal area directly. However, in combination with radiation, it can intensify skin reactions or soreness.
After treatment, monitoring appearance and sensation is important. Some patients notice areas that look different from before treatment, such as smoother or firmer skin, slight discoloration, or residual lumps from scar tissue. These changes do not necessarily indicate cancer recurrence but should still be monitored.
Rehabilitation and follow-up care often include guidance on skin care, hygiene, and managing discomfort. Understanding what to expect post-treatment helps patients distinguish normal healing changes from signs of recurrence. Early intervention and ongoing monitoring remain critical. Awareness of these post-treatment changes can provide reassurance and empower individuals to manage recovery effectively while maintaining anal health and overall well-being.
Prognosis: Why Early Detection Matters
The prognosis for anal cancer is strongly linked to how early it is detected and treated. When caught in its early stages, anal cancer is often highly treatable, and the chances of successful outcomes are significantly higher. Small tumors that have not spread beyond the anal canal or perianal skin respond well to treatments such as surgery, radiation, or combined chemoradiation, with many patients achieving complete remission.
Early detection also minimizes the extent of treatment needed. Smaller tumors often require less aggressive interventions, which reduces the risk of long-term side effects and helps preserve the function and appearance of the anal area. For example, early-stage cancers may be treated with localized surgery or targeted radiation, allowing for quicker recovery and fewer complications compared to advanced disease.
In contrast, late-stage anal cancer, which has grown larger or spread to nearby lymph nodes, can be more challenging to treat. Advanced tumors often require more extensive surgery, higher doses of radiation, or systemic chemotherapy. These treatments may carry greater risks and a longer recovery period. Additionally, advanced disease may affect bowel function or the appearance of the anal area more noticeably.
Timely detection begins with awareness of changes in the anal region, including lumps, sores, persistent bleeding, or discomfort. Regular monitoring, understanding personal risk factors like HPV infection, and seeking prompt medical evaluation when symptoms arise can dramatically improve outcomes.
In summary, recognizing early warning signs and consulting a healthcare professional without delay maximizes treatment success, minimizes complications, and enhances overall quality of life, reinforcing the critical role of early detection in managing anal cancer.
Frequently Asked Questions About Anal Cancer Appearance
People often have many questions about what anal cancer looks like, how it feels, and how to tell it apart from other conditions. Addressing these questions can help reduce anxiety and encourage timely medical evaluation.
Is anal cancer always painful? Not necessarily. Early-stage anal cancer may be painless or cause only mild discomfort. Pain tends to become more noticeable as tumors grow or when they affect deeper tissues. Persistent or worsening pain should be evaluated promptly.
Can anal cancer look like a pimple? Sometimes. Small early-stage tumors may appear as tiny lumps or bumps that resemble pimples or ingrown hairs. The key difference is that cancerous growths usually do not resolve on their own and may slowly increase in size.
Does anal cancer bleed all the time? Bleeding is a common symptom but varies between individuals. Some may notice light spotting, especially after bowel movements, while others may experience intermittent or more significant bleeding. Any unexplained or persistent bleeding should be checked by a doctor.
How fast does anal cancer grow? The growth rate depends on the type and individual factors. Squamous cell carcinoma, the most common type, often grows slowly over months, while more aggressive types can progress faster. Early detection remains crucial regardless of growth speed.
Is itching a sign of anal cancer? Mild itching is common with benign conditions, but persistent or worsening anal itching, especially when accompanied by lumps, sores, or bleeding, may indicate a serious underlying problem and warrants medical evaluation.
Can I check for anal cancer myself? Self-examination can help notice visible lumps, sores, or skin changes, but it cannot reliably detect tumors inside the anal canal. Professional evaluation, including a digital rectal exam and possible biopsy, is essential for accurate diagnosis.
Answering these common questions empowers individuals to recognize warning signs, differentiate them from minor conditions, and seek timely care, which is critical for early detection and successful treatment.
Final Thoughts:
Awareness and early action are the most important tools in managing anal cancer. While it can be uncomfortable to notice changes in such a private area, paying attention to persistent lumps, sores, bleeding, or discomfort is crucial.
Early detection dramatically improves the chances of successful treatment, reduces the need for extensive interventions, and helps preserve the appearance and function of the anal area.
It is also important to remember that not every change signals cancer. Hemorrhoids, anal fissures, warts, or minor skin irritation are far more common.
However, any unusual or persistent symptom that does not improve within a few weeks should not be ignored. Self-monitoring combined with timely medical evaluation ensures that serious conditions are ruled out or addressed early.
Consulting a healthcare professional provides reassurance, accurate diagnosis, and access to appropriate treatment options. Modern treatments, including surgery, radiation, and chemotherapy, are highly effective, especially when initiated in the early stages.
Additionally, follow-up care and monitoring help detect recurrences or complications quickly, giving patients the best possible outcomes.
Lastly, addressing anal health openly, without shame or fear, benefits both physical and emotional well-being. Support from healthcare providers, family, or patient groups can help overcome embarrassment and encourage proactive care.
By listening to your body, observing changes carefully, and seeking prompt medical attention for anything unusual or persistent, you take control of your health and reduce the risks associated with anal cancer. Awareness, vigilance, and early action remain the most powerful strategies for maintaining both anal health and overall well-being.

Jordon Fox is an emerging artist and creative from Philadelphia, Pennsylvania, known for blending music, fashion, and fitness into his personal brand and artistic identity. He’s built a reputation as a multi-talented creator with a strong focus on authenticity and inspiring others.